Implants, Joints, and Stents
Joint replacement, particularly for the hip and knee, has become a common surgical procedure for the treatment of joints affected by arthritis. Joint replacement replaces the surfaces of the natural joint and leads to restoration of joint function and pain relief.
The hip consists of the articulation between the spherical femoral head and the cup-shaped acetabulum. The first total hip replacement was performed in 1938 by Philip Wiles at the Middlesex Hospital in London. The design, made from stainless steel, consisted of a spherical femoral component attached to a bolt passing down the femur and a cup-shaped acetabular part that was secured by screws.
However, it was not until the 1950s and 1960s that the idea of joint replacement became possible through the pioneering work of Kenneth McKee (Norwich, U.K.) and John Charnley (Wrightington, U.K.). McKee had designed a hip replacement, similar to the one used by Wiles, with a stainless steel ball and socket secured by screws. However, the results of replacements were poor because of inadequate fixation.
Charnley developed the idea of using dissimilar materials to create a low friction implant. He used a stainless steel femoral component and plastic socket made from polytetrafluorethylene (PTFE), more commonly know as Teflon. Charnley also introduced the idea of using large amounts of acrylic cement to fix the implant. The cement was used as a grout, relying on the mechanical fit rather than a glue. Over 300 hip replacements were undertaken by Charnley before it was realized in 1962 that PTFE was not a suitable material for hip replacement.
Studies found that high wear rates resulted in a severe tissue reaction. Later in 1962, Harry Craven, the technician at Charnley’s biomechanical laboratory, obtained a new plastic known as high-molecular weight polyethylene (HMWPE). At first Charnley was dismissive of the new material, but Craven tested it on a wear machine and found that it had much lower wear rates than PTFE and appeared to be a better material for hip replacement.
Charnley began implanting the new metal-on-plastic hips in November 1962, and this is the basis of the metal-on-plastic hip implant that was most commonly used up to the twenty-first century. The metal component, however, was often a cobalt chrome molybdenum alloy (CoCrMo), and the plastic was ultra-high molecular weight polyethylene (UHMWPE) (see Figure 3).
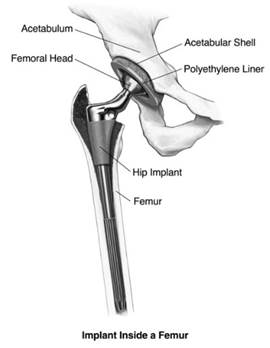
Figure 3. A total hip replacement showing the femoral and acetabular components
Metal-on-polymer hip replacements can be expected to last for at least 15 years, but the wear particles developed from the metal articulating against the polymer leads to wear debris, which can cause osteolysis. Osteolysis is a tissue reaction that causes bone resorption and loosening of the implant, and the problem has led to growing interest in alternative biomaterials for hip replacements. Metal-on-metal (CoCrMo) and ceramic-on- ceramic (alumina) are considered to lead to less wear debris and to avoid the problem of osteolysis.
The knee consists of the articulation between the femur and the tibia; the two bones being separated by fibrous cartilage called the meniscus. In addition the patella (knee cap) articulates with the femur. The development of knee replacements followed a similar trend to that of hip replacements in which early attempts failed, mainly because of loosening. In the early 1950s, hinged knee replacements were developed by Wallidus (1951) and Shiers (1953).
These two implants consisted of a stainless steel hinge, but they required large bone resection, and there were high failure rates associated with them. Modern-day knee replacement took off after the success of the Charnley metal-on-polymer hip replacement. In 1969, Gunston, who worked with Charnley at Wrightington, developed a metal-on- polymer knee replacement that was fixed with acrylic cement. The implant consisted of a stainless steel femoral component and a HMWPE tibial component.
By the end of the twentieth century, there were various designs of knee replacement available that consisted of femoral, tibial, and/or patellar components.
The implant can be:
(1) unconstrained;
(2) semi-constrained; or
(3) fully constrained, depending on whether the knee ligaments are present. Implants are also divided according to the proportion of the knee replaced:
(1) unicompartmental to replace either the medial or lateral compartment;
(2) bicompartmental to replace both medial and lateral components;
(3) tricompartmental to replace medial and lateral components and the patella.
Present-day knee replacement (see Figure 4) consists of a metal femoral component (CoCrMo) that has a stem cemented into the femur, a tibial stem of titanium alloy cemented into the tibia, a tibial tray (UHMWPE) that fits to the tibial stem, and a patellar component (also of UHMWPE).
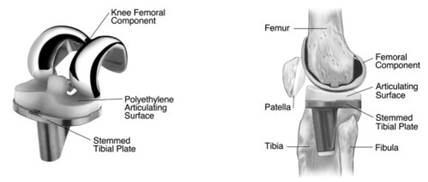
Figure 4. A total knee replacement showing the femoral, tibial, and patellar components
The fixation, or setting, of fractures has been aided by the use of screws and pins. The use of screws in bone began around the late 1840s, and today bone screws are commonly used either alone to treat fractures or in conjunction with plates or intramedullary nails. They are generally made from stainless steel or titanium alloy.
The screws can either be self-tapping (the screw cuts a thread as it is inserted) or non-self-tapping (requires a tapped hole). Two main types of screws are used to get good purchase in the two types of bone: cortical (small threads) and cancellous (large threads). The holding power of a bone screw depends on a number of factors including diameter, length of thread engagement, and thread geometry. Hence, there are many different designs, lengths, and diameters of screw available for fracture fixation. Screws can also be cannulated (have a hole down the center) for use with wires and pins.
Pins or wires are also used in fracture fixation. The use of wires dates to the 1770s. Straight wires are known as Steinmann pins, while wires of diameter less than 2.4 millimeters are known as Kirschner wires. Wires and pins are primarily used to hold bone fragments together, either temporarily or permanently. They can also be used to guide large screws or intramedullary nails during insertion. The pins have a sharpened tip designed to penetrate easily through the bone.
A stent is a device used to maintain an orifice or cavity in the body. Stents are mainly used in vascular diseases to maintain blood flow, although they can be used to maintain a passage in other sites such as the urinary duct or for a bronchial obstruction. The most common type of stent used for coronary artery disease is made from fine stainless steel wire; the device has a lattice appearance resembling chicken wire. In angioplasty procedures, the stent is inserted into the artery on a balloon catheter.
The balloon is inflated, causing the stent to expand and press against the inside of the artery. Once the balloon has been deflated and removed, the stent remains in place keeping the artery open. Other stents can be made from a variety of materials: nitinol (a nickel-titanium alloy), polymers, elastomers, and biodegradable materials.
Date added: 2023-10-26; views: 657;
