Etiology and Pathogenesis of Iron Deficiency in Pregnancy
During pregnancy there is a disproportionate increase in plasma volume, erythrocyte number and hemoglobin mass. Whereas the plasma volume increases by about 40%, the number of erythrocytes and hemoglobin mass increases by about 20% each. Thus, there is an apparent fall in hemoglobin concentration and hematocrit value.
There is a marked extra demand of iron during pregnancy, especially in the second half. The fall in hemoglobin concentration during pregnancy is due to the combined effect of hemodilution and negative iron balance. The woman who has got sufficient iron reserve and is on balanced diet is unlikely to develop anemia during pregnancy in spite of increased demand for iron.
But if the iron reserve is inadequate or absent, the factors which lead to the development of anemia during pregnancy are:
- increased demands for iron;
- diminished intake of iron (apart from socioeconomic factors, the inadequate dietetic habits, loss of appetite and vomiting in pregnancy are responsible factors);
- disturbed metabolism;
- pre-pregnant health status;
- abnormal demand: multiple pregnancy increases the iron demand twofold. Women with rapidly recurrent pregnancy, within 2 years following the last delivery, need more iron to replenish deficient iron reserve.
Iron deficiency occurs when the level of stored iron becomes depleted. Iron deficiency anemia occurs when iron levels are sufficiently depleted to produce anemia. In Iron deficiency anemia there is shortage of iron stores (low ferritin), reduced transport and functional iron (low transferrin), limiting red cell production e.g. reduced Haemoglobin (Hb).
The group of patients with a higher risk of anemia in pregnancy includes:
- women with extragenital diseases (rheumatism, cardiac diseases, chronic pyelonephritis, gastroenteritis, diabetes, chronic tonsillitis, liver diseases, etc);
- multiparae;
- women in which this pregnancy occurred in the period of lactation;
- women, in which the previous pregnancy was complicated with preeclampsia-eclampsia syndrome, hemorrhages, anemia;
- women, in which this pregnancy is complicated with hemorrhages, threatened abortions, preeclampsia-eclampsia syndrome, viral infections;
- women with mulnutrition
Risk factors for iron deficiency or IDA in pregnant women also include an iron-deficient diet, gastrointestinal issues affecting absorption, or a short pregnancy interval.
Effect of anemia on pregnancy.Severe or untreated iron-deficiency anemia during pregnancy can increase the incidence of following complications in pregnancy:
- Complications to the fetus
- Intrauterine fetal growth restriction
- Low-birth-weight baby
- A preterm birth
- Neonatal anemia
- Impaired psychomotor/mental development of a child
- Complications to the mother:
- Mother may need in blood transfusion (in severe cases)
- Increase risk for hemorrhage in labor and postpartum
- Postpartum depression
- Increased susceptibility of maternal organism to infections
Untreated folate deficiency, as well as vitamin B12 deficiency, can increase risk of having a:
- Preterm or low-birth-weight baby
- Baby with a serious birth defect of the spine or brain (neural tube defects).
Effective management is needed to prevent adverse maternal and pregnancy outcomes, including the need for red cell transfusion.
There is ambiguous information regarding the Hb threshold below which mortality increases, but it is known that severe anemia is associated with a doubling of the maternal death risk. Severe anemia with maternal Hb levels less than 70 g/L has been associated with abnormal fetal oxygenation resulting in nonreassuring fetal heart rate patterns, reduced amniotic fluid volume, fetal cerebral vasodilatation, and fetal death. Thus, maternal transfusion should be considered for fetal indications.
Effect of Pregnancy on anemia. Pregnancy is characterized by an increased need of the mother's body in iron, folates, vitamins due to the growing fetus and placenta. Thus, the pregnant women are at a higher risk of developing anemia due to excess blood that the body produces in order to help provide nutrients for the baby, and because of the increased demand for iron. The woman, suffering from anemia before pregnancy already has lack of the level of stored iron, and in pregnancy she has significant risk for progressive worsening of the course of anemia.
Symptoms of anemia during pregnancy. The most common symptoms of anemia during pregnancy are:
- Pale skin, lips, and nails
- Feeling tired or weak
- Dizziness
- Shortness of breath
- Rapid heartbeat
- Trouble concentrating
Diagnosis. The diagnosis of iron deficiency anemia is based on chief complaints, data of thoroughly taken history, estimation of objective status, data of laboratory research. At the objective inspection, the pallor of skin and mucous membranes is marked. On heart auscultation the muffled I tone and slight “anemic” systolic murmur on the apex and pulmonary artery are marked.
On history taking special attention is paid to feature of nutrition, state of gastrointestinal system, past illnesses, number and the course of pregnancies in her anamnesis, multiple pregnancies, bleedings at previous deliveries and in postpartum period, the duration of lactation, and availability of occupational hazards.
The basic laboratory indexes allowing to diagnose the state of iron deficiency are the level of hemoglobin, color index, quantity of erythrocytes and reticulocytes, hematocrit and serous iron.
Lab tests:
· CBC (Complete Blood Count) below 110g/l at booking and below 105g/l at 28 weeks indicates anemia. There is often a low MCV (microcytic), low MCH (hypochromic) anemia with iron deficiency, although microcytic hypochromic anemia can also indicate hemoglobinopathies.
· Serum ferritin. This is the first laboratory test to become abnormal in iron deficiency and is the most useful and easily available parameter for assessing iron deficiency (< 30 microgm/L). Serum Ferritin is not performed routinely unless there is a lack of response to (2-3 weeks) trial of oral iron, or before IV iron administration, or to assess response to treatment.
· Other tests like serum iron, total iron binding capacity lack sensitivity and specificity and hence are not recommended in routine diagnosis.
Three degrees of iron deficiency anemia are distinguished depending on degree of deficiency: mild, moderate, severe (Table 21).
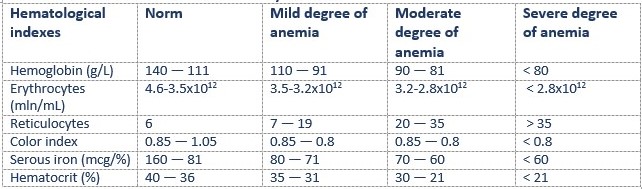
Table 21. Classification of Iron Deficiency Anemia
Management. Maternal iron requirements average 1000 mg/d. Because many pregnant women lack sufficient iron stores, iron supplementation may be included in prenatal care. Primary prevention for average-risk populations includes adequate intake of dietary iron and oral, low-dose (30 mg/d) iron supplements early in pregnancy. Suggested prophylaxis for IDA in high-risk populations is 60 to 100 mg of elemental iron daily.
All pregnant women should be screened for anemia, and those with iron deficiency anemia should be treated with supplemental iron, in addition to prenatal vitamins.
A routine antenatal check-up with blood examination before 10 weeks of pregnancy is carried out in patients form the group of higher risk of IDA. The revealing of the 3 degree of anemia in early stages of pregnancy may be an indication for medical abortion. After 12 weeks of pregnancy the question of therapeutic abortion should be solved individually depending on age of pregnant, data of anamnesis and concomitant obstetric and extragenital pathology. In other cases pregnancy should be prolonged till the term of delivery, the examination of blood should be carried out regularly, and treatment should be administered to prevent a progressive anemia.
Patients with Hb concentration ≥110 g/L and the serum ferritin concentration >20 µg/L usually not need in iron medication, but need in accurate regular screen for anemia and a diet enriched with iron. A varied diet of iron-rich foods and foods that enhance iron absorption (meats and ascorbic acid-rich fruits) should be recommended to the patient. Items that inhibit absorption of iron (tea, coffee, whole-grain cereals, particularly bran, unleavened whole-grain breads, and dried beans) should be consumed separately from iron-rich foods.
Pregnants with a mild degree of anemia are usually treated at the out-patient department, in antenatal clinic. When the Hb concentration is between 90 and 109 g/L and the serum ferritin concentration is between 12 and 20 µg/L, or the Hb concentration is ≥110 g/L and the ferritin concentration is ≤20 µg/L, supplemental iron should be administered by 30 mg daily.
60-120 mg of supplemental iron should be administered by mouth when the Hb concentration is between 90 and 109 g/L and the ferritin concentration is
Medical treatment at the in-patient department is indicated in the following cases:
· anemia of a moderate and severe degree (in the late terms of pregnancy);
· inefficiency of out-patient therapy;
· presence of accompanying extragenital pathology;
· presence of obstetric complications. (table 21)
Table 22. Medicines for oral treatment in pregnancy
Parenteral iron therapyshould bereserved for patients who are either unable to absorb oral iron or who have increasing anemia despite adequate doses of oral iron. (Table 22)
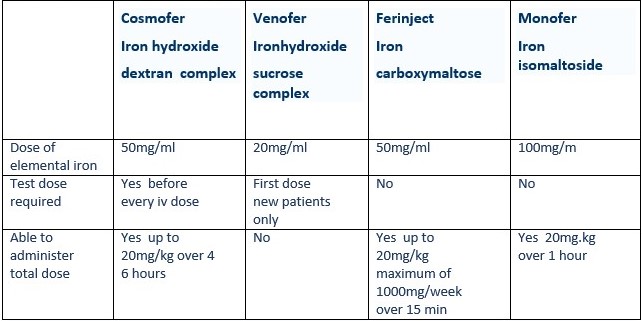
Table 22. Parenteral iron therapy
Pregnants with anemia should be hospitalized at the in-patient department 2 weeks before labor to plan an obstetric management and preparation to birth.
The most preferable type of delivery for patients with anemia is delivery through the natural maternal passages, with prophylaxis of weakness of labor pains, fetal hypoxia and asphyxia of neonate. The 3rd stage of labor should be conducted with a needle in the vein; 1 ml of methylergometrine should be injected during crawning of the head (in multiparae) or disengagement of the fetal head (in primiparae). The obstetrician should be ready for manual control of the uterine cavity during labor. After delivery the puerperal septic diseases are common for these patients, so their prophylaxis should be carried out. The treatment of iron deficiency should be continued in postpartum period.
For women, whose pregnancy was complicated with anemia, the next pregnancy may be recommended not earlier than in 2-3 years.
Pregnancy and Thrombocytopenias. Thrombocytopenias are a group of diseases, at which the number of thrombocytes is lower than the existing norm — 150х109/l — 400х109/l. The decrease of thrombocyte quantity can be caused by their increased destruction, elevated consumption and insufficient formation.
The hereditary and acquired forms of thrombocytopenias are distinguished. At hereditary forms the change of functional properties of thrombocytes takes place that gives grounds to refer them to the group of thrombocytopathies.
Acquired forms of thrombocytopenias are divided into:
· Immune forms;
· Forms caused by mechanical traumas of thrombocytes (at hemangiomas, splenomegaly);
· Suppression of cell proliferation of bone marrow (at aplastic anemia, chemical and radiation damage of bone marrow);
· Replacement of bone marrow by a tumor tissue (at Marchiafava-Micheli disease);
· Increased consumption of thrombocytes (at thromboses, syndrome of disseminated intravascular coagulation);
· Vitamin B12 or folic acid deficiency.
The most common form encountered in obstetric practice is the idiopathic Werlhof's disease, which is in 90 % of cases is the acquired autoimmune form of thrombocytopenia. Werlhof's disease is the common name of thrompocytopenias, which are not connected with acute leucosis, Marchiafava-Micheli disease, vitamin B12 or folic acid deficiency. In case of Werlhof's disease the quantity of megakaryocytes is increased, while the size of spleen is normal.
Pathogenesis. The insufficient quantity of thrombocytes and related to it reduction of thrombocyte’s component in the system of blood coagulation is the basis of pathogenesis of the disease. The decrease of quantity of circulating thrombocytes is connected with duration of their life which shortens to several hours instead of 7-10 days. The reasons of destruction of thrombocytes on the periphery are antibodies to circulating thrombocytes.
It is known that thrombocytes participate in maintenance of a normal condition of endothelium of microvessels, form primary thrombocytic plaques at damage of vessels, participate in blood coagulation and are one of inhibitors of fibrinolysis. The thrombocytes take a leading role in bleeding arrest in a zone of microcirculation (primary hemostasis), whereas the formation of fibrinous clots occurs later (secondary coagulatory hemostasis).
At thrombocytopenia hemorrhagic diathesis has a microcirculatory character and occurs due to increased fragility of vessels, as well as due to escape of erythrocytes from bloodstream via capillaries (bleeding per diapedesin).
Clinical Picture. Acute, subacute and chronic forms of disease are distinguished.
Clinically the disease is manifested by hemorrhages from fine vessels of the skin and mucous membranes. Petechial hemorrhage occurs on the skin at slightest traumas: taking somebody's blood pressure, rubbing of skin in places of injections, at palpation. The patients can be disturbed by bleedings: nasal, gastrointestinal, metrorrhagia, etc., especially frequent at severe forms of disease.
On investigation of peripheric blood the decrease of thrombocyte quantity up to 50-40 х109/l, down to their complete disappearance is marked. There are gigantic forms of platelets in peripheric blood. The quantity of plasma elements of blood is normal; sometimes even increase of quantity of factors of blood coagulation is possible, apparently of a compensatory character. The level of haemoglobin and erythrocytes can be normal or, owing to bleedings, reduced. The duration of bleeding by Duke (Duke’s test) is lengthened, while coagulatory hemostasis (time of blood coagulation) can be not disturbed or even slightly accelerated (at compensated forms). The retraction of a bloody clot is impaired.
Aggregative properties of thrombocytes and their adhesion can be reduced due to sharp decrease of quantity of circulating thrombocytes. Diagnostics of disease is possible at a sternal puncture to exclude hemoblastoses, Marchiafava-Micheli disease, cancer metastases, etc. The normal content of megacaryocytes in a punctate of the bone marrow is characteristic of idiopathic purpura.
Date added: 2022-12-25; views: 832;
