Threatened Preterm Labor
Threatened PTL defined as appearance of uterine contractions (irregular uterine contractions with <2 contractions per 10 minutes) in the absence of critical cervical changes.
The main clinical symptoms are: increase of uterine tone, pain in the lower abdomen (dull, cramping, irregular), low position of the fetal presenting part, blood spotting, premature rupture of amniotic membranes, shortened uterine cervix, dilation of the cervical canal to less than 3 cm. The diagnosis of premature labor should be made even if the patient has one of those symptoms.
Diagnosis of TPTL
1.Assessment of risk factors
2.Vaginal examination to assess the cervical status
3.Ultrasound visualization of cervical length and dilatation
4.Detection of fetal fibronectin in cervicovaginal secretions
Assessment of risk factors: interrogation of a patient, taking a previous history data, evaluation of patient complains, accurate physical examination. A patient who has previously given birth to a premature infant faces a 20 % to 30% risk of recurrence in the next pregnancy, so careful analysis of the previous history, health in whole will help to find risk factors and prevent the onset of premature labor.
Physical examination of a pregnant woman include general appearance and nutrition, blood pressure, pulse, height to weight profile, present weight; head and neck, heart and lungs, breasts, abdomen, pelvic area tenderness, extremities and back, and pelvic evaluation - speculum and bimanual examination, clinic pelvimetry.
Vaginal examination: speculum and bimanual examination are used to evaluate cervical status: its color, external os, consistency, length, dilatation (if any) and position according to the pelvic axis. It also helps to diagnose and evaluate any prior injury to the cervix. A cervical length of 25 mm or less before 37 weeks is suspicious for preterm labor. Cervical effacement and lower uterine segment changes may predate cervical dilatation. Cervical dilatation may be diagnosed with marked accuracy up to 4 cm. Cervical length may be a useful predictor of the risk of premature delivery, with a shorter cervix predicting a higher risk. (Fig.168)
Fig. 168. Cervical status
Ultrasound visualization of cervical length and dilatation: cervical length is most accurately measured by transvaginal ultrasound (TVUS) examination. The cervical length (CL) is usually measured when the bladder is empty. The length of the cervix is measured from its internal opening on the inside of the uterus to its external opening into the vagina. Normally the cervix is about 35 to 48 mm long at 24 weeks. The cervix is considered to be short if the length of the cervix is less than 25 mm long before term (37 completed weeks). The cervix is considered to be very short if the length of the cervix is less than or equal to 20 mm term of labor. (Fig.169)

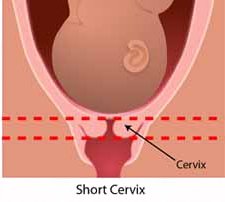
Fig. 169. Cervical length
Fetal fibronectin (FFN) is an extracellular matrix glycoprotein, localized between chorion and decidua. It is present throughout gestation in all pregnancies. It is a diagnostic test for detecting potential preterm labour. The fetal fibronectin test is one of the best predictors to assess risk of preterm labor and preterm birth, by measuring amount of fetal fibronectin in cervico-vaginal secretions. For women with the signs and symptoms of preterm labour without advanced cervical dilatation, a negative FFN result indicates that 96.7% of the patients will not deliver within 7 days and a positive test indicates that 12.7% might deliver within next 7 days.
In normal pregnancies, FFN levels are high (100 μg/ml) during the first 16 to 22 weeks of gestation, and then they fall to very low levels, and rise again (30 μg/ml) as the pregnancy approaches term. However, FFN is not normally detectable (at high levels) in cervico-vaginal secretions between the 22nd and 37th week of gestation. The presence of FFN at high levels during this period may indicate disruption of the uteroplacental interface and has been associated with the preterm birth within 7days from testing.
Contraindications for fetal fibronectin testing:
- Congenital abnormality in fetus
- Cervical cerclage
Accurate identification of women truly in preterm labor allows appropriate application of interventions that can improve neonatal outcome: antenatal corticosteroid therapy, group B streptococcal infection prophylaxis, tocolysis for arresting of uterine contractions, and transfer to a facility with an appropriate level nursery (if necessary). , and transfer to a facility with an appropriate level nursery (if necessary).
Other investigations are also used in diagnosis of TPTL:
- Full blood count (to look for hemoglobin, WBC, platelets, etc.)
- Determination of blood groups, RH factor (patient might need transfusion)
- Full and microscopic examination of urine (urine feme): to assess renal function in general.
- Wet mount for evaluation of vaginal ecology.
- High Vaginal Swab (HVS) for evaluation of vaginal discharge for culture and sensitivity.
Date added: 2022-12-25; views: 728;
