Diseases of a Newborn. Asphyxia Neonatorum
Birth asphyxia is impaired respiratory gas exchange between mother and infant during labor. Synonims: perinatal asphyxia, birth asphyxia. The pathiology refer to the period not only immediately before birth and throughout labor, but also birth itself and the immediate postpartum period, generally thought of as the period of stabilization right after birth. However, a newborn with asphyxia does not breathe spontaneously and may die, thus immediate resustitation is reguired to prevent death or brain damage.
Incidence. The incidence of asphyxia neonatorum lies between 3–5 infants per 1000 live births (4.6/1000). Pathophysiology of asphyxia neonatorum
Perinatal asphyxia results from compromised placental or pulmonary (lung) gas exchange. As a result, hypoxia (lack of O2) and hypercapnia (increased CO2) in the blood develop. Prolonged and severe hypoxia lead to acidosis in the blood due to breakdown of glucose or conversion of glucose in the absence of O2 (anerobic glycolysis), followed with lactic acid production, first in muscle and heart and then in the brain. Lack of sufficient blood flow (ischemia) to all or a part of an organ can be both a cause and a result of hypoxia.
Hypoxia and acidosis can depress heart muscle (myocardial) function, leading to hypotension and lack of sufficient blood flow (ischemia). Systemic hypotension and decreased heart’s pumping power can further compromise and disrupt delivery of substrate and removal of metabolic and respiratory products (eg, lactic acid, carbon dioxide). Thus, the functioning of vital organs and systems in a newborn is disrupted, which is accompanied by typical clinical symptoms.
Risk factors:
· Hypertensive disorders in pregnancy;
· Extragenital diseases with pregnancy (anemia, obesity, diabetes mellitus, heart diseases, etc);
· Placental abruption;
· Placenta previa, vasa previa;
· Placental insufficiency in pregnancy (IFGR, intrauterine fetal distress);
· Fetal anemia (eg rhesus incompatibility);
· Postmaturity;
· Complicated labor (labor induction, CPD, abnormalities of labor pains, etc.);
· Congenital defects of a fetus (a diaphragmatic hernia, Fallot diseases, etc);
· Congenitaldefects, such as a diaphragmatic hernia;
· Anesthetics or analgesics agents, administered to the mother;
· Forceps or vacuum extraction;
· Breech or abnormal presentation;
· Cesarean section;
· Cord prolapse/compression;
Clinical features. Perinatal asphyxia may result in fetal demise, neonatal death, or a period of recovery during which there is organ dysfunction with possible long-term effects, particularly in neurological function. Clinical manifestations of perinatal asphyxia include
• Failure of spontaneous inbreath/respiration;
• Bluish or gray skin color (cyanosis);
• Slow heartbeat (bradycardia);
• Stiff or limp limbs (hypotonia);
· Depression of the neonate at birth (lack of pulmonary, heart functioning, acidosis, ischemia, etc:
· Hypoxic ischemic encephalopathy (HIE),
· Renal compromise with oliguria and elevated creatinine;
· Hypoxic cardiomyopathy (ECHO or ECG abnormality);
· Pulmonary complications including respiratory distress and persistent pulmonary hypertension of the neonate;
· Disseminated intravascular coagulation;
· Hepatic failure;
· Necrotising enterocolitis;
· Fluid overload, hyperkalaemia, hypoglycaemia, and acidosis.
Clinically asphyxia neonatorum is recognised as a condition in the neonate where there is the following combination:
- An event or condition during the perinatal period that is likely to severely reduce oxygen delivery and lead to acidosis,
- A failure of function of at least two organs (may include lung, heart, liver, brain, kidneys and hematological) consistent with the effects of acute asphyxia.
Diagnosis. The diagnosis of neonatal asphyxia,delivered on the basis of clinical symptoms is late diagnosis. At present, the assessment should include a history of maternal and intrapartum risk factors for problems that may affect the infant including pre-existing medical conditions in the mother, problems of pregnancy, abnormalities identified antenatally in the fetus, the presence of meconium stained liquor, CTG abnormalities, scalp pH, maternal indicators of infection, presentation and method of delivery. Predictive factors in labor should be evaluated:
•Intrauterine fetal distress in pregnancy, undependent on the term of pregnancy, evaluated by CTG, Doppler investigation, BBP in pregnancy and labor
•Expulsion of meconium-stained amniotic fluid;
•Fetal Tachicardia (>160BPM);
•Or Bradicardia
Management of a newborn with birth asphyxia. After birth all infants must be quickly dried in a warm towel and then placed in a second warm, dry towel before starting resuscitation. This prevents rapid heat loss due to evaporation. Handling and rubbing the newborn infant with a dry towel is usually all that is needed to stimulate the onset of breathing. Stimulation alone will start breathing in most infants.
If the infant fails to respond to stimulation, then the infant must be actively resuscitated. There are 4 main steps in the basic resuscitation of a newborn infant. They can be easily remembered by thinking of the first 4 letters of the alphabet, i.e. "ABCD" - Airway - Breathing - Circulation - Drugs. One of the main principles of ABCD-resuscitation is the regular check up of the patient’s condition. Assessment of Apgar scale is not practical for this purpose. Currently, in the process of resuscitation of newborn it is necessary every 30 seconds to evaluate 3 signs: respiration rate, heart rate, color of the skin in order to determine the next steps of resuscitation.
Step 1 (Airway) - open and clear the airway. Open the airway by placing the infant’s head in the neutral position with the neck slight extended. Do not flex or over extend the neck.(Fig. 236)
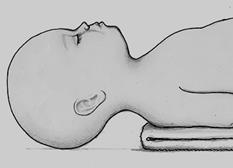
Fig. 236. Infant with head in neutral position
Gently clear the throat. The infant may be unable to breathe because the airway is blocked by mucus or blood. Therefore, if the infant fails to breathe after stimulation, gently suction the back of the mouth and throat with a soft F 10 catheter. Excessive suctioning, especially if too deep in the region of the vocal cords, may result in apnoea and bradycardia by stimulating the vagal nerve. This can be prevented by holding the catheter 5 cm from the tip when suctioning the infant's throat. Do not suction the nose before suctioning the mouth or throat as this often causes the infant to gasp: suction the mouth first, then the baby’s nose (‘m’ before ‘n’).
The 1st step (drying, positioning, suctioning, tactile stimulation) should take approximately 20-30 seconds. After drying, positioning, suctioning, tactile stimulation of a newborn assessment of neonatal respiration is needed again.
If no meconium in the amniotic fluid after suction mucus from the mouth and nose, and if the newborn is crying and breathing is normal, no resuscitation is needed.
If the infant still fails to breathe adequately, artificial ventilation (initially with Ambue mask) is required.
If meconium is present in the amniotic fluid after suction mucus from the mouth and nose, it is necessary to suck mucus from the throat with an endotracheal tube introduced using a laryngoscope.
If the heart rate is
Step 2 (Breathing) - start the infant breathing by providing adequate ventilation.
Mask ventilation: The mask must be held tightly over the infant's nose and mouth. Make sure the head is in the correct position and the airway is clear. Adequacy of ventilation is assessed by observing the chest movements. After effectively ventilating for about 1 minute, stop briefly but do not remove the mask and bag and look for spontaneous breathing. If there is none or it is weak, continue ventilating until spontaneous cry/breathing begins. If the newborn starts crying stop ventilating but do not leave the newborn. Even if breathing is not started, most infants can be kept alive with face mask ventilation until help arrives.
Intubation and ventilation: the most effective method of artificial respirationis is ventilation is via an endotracheal tube. Intubation and ventilation are needed if adequate chest movement cannot be achieved with mask ventilation.Infants who fail to respond to mask ventilation must be intubated. Ventilate the infant at a rate of about 40 breaths a minute. Make sure that the infant's chest moves with each breath and that good, bilateral air entry is heard. Adequate ventilation is the most important step in resuscitating an infant with neonatal asphyxia.Every 30 seconds check up 3 signs: breathing, heart rate, skin color.
Step 3 (Circulation) - obtain a good circulation with chest compressions.
Apply chest compressions (external cardiac massage) at about 80 times a minute if the heart rate remains below 60 beats per minute after effective ventilation has been started. Place the fingers of one or two hands under the infant's back and press on the lower half of the sternum with your thumb or thumbs. Usually two chest compressions are followed by a breath.
2 techniques of indirect cardiac massage are used:
thumbs method - press the breast by pads of two thumbs, while the rest of the fingers of both hands support the child back (this method is preferred)
two fingers method - press the breasts by tips of two fingers of one hand: the second and third or third and fourth, during this second hand supports the child back (Fig. 237). This method is used if access to the vessel umbilical cord is needed
Fig. 237. Indirect cardiac massage by the method of two fingers
Step 4 (Drugs) - start medications if needed. Indications for the use of drugs: despite adequate ventilation by 100% oxygen and indirect cardiac massage for 30 seconds, the heart rate remains 60 – 80 for 1 minute. A special solution of adrenalin should be prepared immediately for infant: 0.1 ml of a 0.1% solution of adrenalin in combination with 0.9 ml of 0.9% solution of natrium chloridum. 0.2 ml/kg of body weight of this mixed solution should be injected intravenously for treatment of infant in case of bradycardia with 100 beats per minute. This injection may be repeated in 5 minutes intravenously or endotracheally. In case of significant bradycardia (less than 80-60 beats/minute), intracardiac injection of adrenalin should be done immediately.
Every 20 seconds 3 signs (natural respiration, heart rate, colour of the skin) should be evaluated to determine the effect of treatment.
After the occurrence of natural respiration and normalizing heart rate, oxygen inhalation should be continued until the skin becomes pink.
Infections of Newborn. The fetus normally synthesizes only very small amounts of immunoglobulins. However, after the twentieth week of gestation the intrauterine infections such as syphilis, rubella, cytomegalovirus infection and toxoplasmosis will stimulate the production of fetal IgM and IgA. The presence of a raised level of non-specific IgM antibody in the baby therefore suggests some kind of prenatal infection, at term baby cord levels of IgG are similar to those of maternal blood thus passively transferred antibody gradually disappears over the first few months of life. In "preterm” babies (of 32 weeks and less) placental transfer is not so efficient and their serum levels of IgG are low for the first three months of life. In a newborn baby phagocytosis is less efficient than normal and this contributes to the increased susceptibility to bacterial infection. Breast feeding confers some immunological advantages, particularly the transfer of IgA.
Sources of Infection. During pregnancy such organisms as rubeola virus and cytomegalovirus reach the fetus from the mother through the placenta. During birth the baby may be directly infected with organisms present in the birth canal and these include gonococci, group В streptococci and E. coli. After birth the infections with staphylococci, streptococci and blue pus bacillus (Pseudomonas aeruginosa) are derived from the environment.
Colonization of umbilicus, nose, throat and rectum takes place over the first few days of life. The organisms found in these sites are usually Gram-negative (E. coli and Ps. aeruginosa) in low-birth-weight infants, and Gram-positive (streptococci and staphylococci) in normal full term infants.
Clinical Features. The presenting symptoms and signs of neonatal infection are usually non-specific, especially in low-birth-weight babies or those who are already ill for other reasons. Lethargy and reluctance to feed are the first and the only indication of infection. Fever may be present but the temperature may be normal or even subnormal; the baby's colour is unnatural, it may be cyanosed or pale or even jaundiced. The liver and spleen are often enlarged. The infection is probably advanced. There may be fits and a bulging fontanelle in meningitis and rapid grunting respirations in pneumonia.
Laboratory Investigations. The object of investigation is to confirm the presence of infection, to localize its site and to determine the identity and sensitivities of the infecting organism. Blood, swabs and other material should be cultured. White cell counts may be helpful if the total count is about 7,000 per cm3 after the fourth day of life with a marked shift left in the neutrophils. Serum levels of IgM are raised in the newborn following intrauterine infections so that a risen level after birth does not provide evidence of a postnatal infection.
Date added: 2022-12-25; views: 735;
