Emergency Treatment of Some Specific Causes of Shock in Obstetrical Practice
Hypovolemic shock. Hypovolemic shock may result from loss of whole blood, plasma, or fluid and electrolytes.
In many patients with hypovolemic shock who are seen in the emergency department, the cause of shock will be immediately apparent, eg, obvious bleeding or history of severe diarrhea.
Diagnosis. The clinical features of shock are present. In addition, there may be signs suggesting hypovolemia as the cause, for example, of obvious hemorrhage or clinical features associated with volume loss due to burns, peritonitis, premature separation of normally located placenta, placenta previa. Central venous pressure is low, and both venous and arterial pressure improves rapidly with intravascular volume replacement.
Treatment. Place the patient in a recumbent position. Give oxygen by nasal prongs or mask.
Gain intravascular access. The number of intravenous cannulas required depends on the severity of shock. Catheters may be inserted either by venous cutdown or by percutaneous method. The safest site for a venous cutdown is the saphenous vein at the ankle. If shock is not severe and the vein is not collapsed, insert a 16-gauge percutaneous catheter. The basilic vein in the antecubital fossa is also a good site for a large-gauge percutaneous catheter or venous cutdown. If an individual is attempting resuscitation without assistants, a temporary percutaneous catheter inserted in the femoral vein may permit rapid access to the circulation without major complications.
As about catheterization of central veins: avoid percutaneous catheterization of the subclavian or jugular veins for treatment of hypovolemic shock, since the great veins are usually collapsed, and the chances of complications such as hemothorax and pneumothorax are greatly increased. For a patient in hypovolemic shock, the additional insult of hemothorax or tension pneumothorax may be rapidly fatal.
Administer intravenous fluids at once to restore adequate intravascular volume. The goal is normal cardiac output and tissue perfusion.
Types of fluids. Table 15 lists various solutions used in resuscitation of patients in shock. These solutions may be divided into 2 main types: crystalloids and colloids.
a. Crystalloids: they include isotonic saline and balanced salt solutions (lactated Ringer’s solution, Acetated Ringer’s solution, Acesol, Disol, Treesol, Lactasol.
Balanced salt solutions contain varying amounts of acetate or lactate (or both) that are metabolized to bicarbonate when there is adequate perfusion of the liver. Crystalloids have the advantages of being readily available and relatively inexpensive.
b. Colloids: they contain high-molecular-weight substances that do not easily diffuse across normal capillary membranes. This property may enable these fluids to be retained longer in the intravascular space. Colloid solutions also cause an increase in plasma oncotic pressure, which should draw fluid from the interstitial space into the intravascular space to cause additional volume expansion. Both of these properties should prevent accumulation of pulmonary interstitial fluid that would hinder oxygen diffusion. Capillary membranes are often damaged in the patients in shock, however, so that larger molecules (form the high-molecular-weight substances) may leak from the intravascular space into the interstitium, where they could theoretically have an adverse effect on pulmonary function. Common colloid solutions include the following:
c. Blood. It is most commonly available as packed red blood cells or whole blood. In patients with mild hemorrhagic shock, especially if blood pressure can be maintained with asanguineous fluids, typed and cross-matched packed red blood cells are preferred. Whole blood should be used as soon as possible in patients with moderate to severe hemorrhagic shock. Blood should not be given to patients with hypovolemic shock in whom the hematocrit is higher than 30-35%.
d. Plasma or albumin solutions. They are effective volume expanders; however, they are expensive and may be harmful if they enter in pulmonary interstitium as a result of capillary leakage. They may also transmit infectious agents (the same whole blood). The authors feel, therefore, that plasma and plasma products should not be used until capillary integrity has been regained.
e. Plasma substitutes. Plasma substitutes such as dextrans have been used for initial volume replacement in hypovolemic shock.
Choice of fluids. The choice of fluid for resuscitation depends on the type of hypovoemic shock present (hemorrhagic versus nonhemorrhagic) and on the severity of shock.
a. Mild shock. Normal saline, lactated or acetated Ringer’s injection, and plasma or other blood products are equally effective in treating patients in mild shock. Crystalloid solutions are strongly preferred because of their low cost, lack of adverse effects, and ready availability.
b. Moderate to severe shock. Considerable controversy exists regarding the correct fluid to use in patients with moderate to severe shock. Some authorities feel that colloids are associated with fever adverse pulmonary effects than crystalloids in patients with severe shock, whereas other authorities feel that colloids are potentially more harmful than crystalloids. A recent review suggests that crystalloids and colloids probably have equivalent effects if the amounts given achieve the same hemodinamic end points. The authors generally recommend crystalloids because of their low cost and lack of adverse effects.
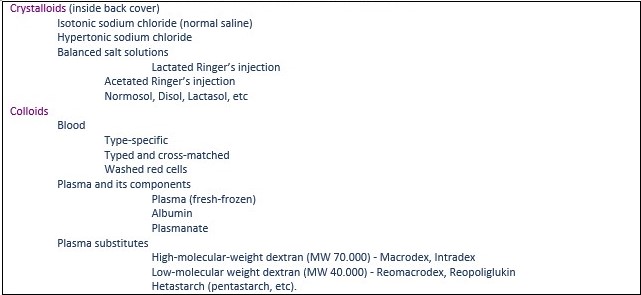
Table 27. Fluids used for resuscitation of the patients in shock
c. Hemorrhagic shock. Isotonic saline or one of the balanced salt solutions should be used for initial resuscitation, because these substances are cheap and readily available, and they effectively restore vascular volume for short periods. As much as 2-3 l of crystalloid solution may be given to maintain adequate blood pressure for the 30-40 minutes required for definitive cross-matching of blood. As noted above, patients in mild hemorrhagic shock can be treated with cross-matched packed red cells, whereas patients in moderate to severe shock should receive whole blood.
d. Nonhemorrhagic shock. Hypovolemic shock due to dehydration or third-spacing should be managed with crystalloid solution alone.
Evaluate the effectiveness of resuscitation:
1. Monitor indices of resuscitation: The best indicators of successful resuscitation are improved atrial filling pressures and improved urine output. Additional guidelines include improved state of consciousness and peripheral perfusion (as measured by clinical criteria including arterial blood pH). In an intensive care unit setting, measurements of cardiac output are also useful.
a. Atrial filling pressure: The only estimate of atrial filling pressure available in most emergency departments is the central venous (right atrial) pressure. It is generally a good measure of intravascular volume but may be unreliable in patients with cardiac or pulmonary disease or in those who require mechanical ventilatory support. Such patients require measurement of pulmonary capillary wedge pressure, a procedure that should be performed only in an intensive care unit.
Atrial filling pressure should be kept at or near normal levels (3-8 cm water), especially if there is severe shock associated with pulmonary capillary leakage. Filling pressure higher than 3-8 cm water may cause or exacerbate pulmonary edema.
b. Urine output: Urine output is a good index of visceral blood flow (specifically, renal blood flow) and should be maintained at more than 0.5 ml/kg/h. This measurement is unreliable in patients with preexisting serious renal damage or when renal damage has occurred as a result of prolonged shock.
2. Record progress of resuscitation: Documentation, preferably entered on an emergency department critical care flow sheet is essential both for emergency department management and for later management once the patient has been transferred to an intensive care unit or operative room. The following information should be systematically recorded:
a. Vital signs – Record blood pressure, pulse, and respiration rate every 5-15 minutes.
b. Fluids – Note the quantity and type of fluid administered.
c. Central venous pressure – measure and record central venous pressure every 30-60 minutes or as dictated by the progress of resuscitation.
d. Urine output – Measure urine output (with an indwelling catheter), and record it every 30-60 minutes.
e. Other factors – Obtain and record serial hematocrits, arterial blood gas determinations, electrolyte measurements, and renal function tests as indicated.
Aggressively search for the cause of persistent shock: Persistent shock in a patient who initially responded to treatment suggests ongoing, often occult hemorrhage. Obtain serial hematocrit measurements, give whole blood, and search for hidden sources of blood loss. Patients with severe, refractory shock may require immediate surgery (left thoracotomy to cross-clamp the aorta; exploratory laparotomy). Possible sources of blood loss include the following:
a. Abdomen. Hidden blood loss in the abdomen is common. Distension is a late and unreliable sign. Intraabdominal hemorrhage must be assumed to be present in any patient in shock who has a normal chest x-ray and no external signs of significant bleeding. Diagnostic peritoneal lavage may be helpful if gross blood is found or if a hematocrit of 2% or more is noted on the lavage sample. Absence of these signs does not exclude the possibility of intraabdominal bleeding. A computed tomography (CT) scan may demonstrate intraperitoneal fluid and help identify injury to specific solid organs. Its use should be restricted to patients who are relatively stable and for whom it can be obtained rapidly.
b. Retroperitoneum. Bleeding in the retroperitoneum cannot be diagnosed with routine studies. A computed tomography scan is a helpful diagnostic aid if the patient’s condition is stable enough to permit this delay.
c. Pelvis. The pelvis may conceal a large amount of blood; hemorrhagic shock is a common sequela of pelvic fracture, injuries of pelvic organs, etc.
Date added: 2022-12-25; views: 760;
