Detection, Diagnosis, and Assessment of Alcohol Use Disorders
Diagnosis is the first step in the selection of treatment for persons with alcohol use disorders. Diagnosis not only includes the core syndrome of alcohol dependence, but also related conditions such as alcohol withdrawal and comorbid medical and psychiatric disorders. Diagnostic criteria for alcohol use disorders are described in the International Classification of Diseases, 10th edition (ICD- 10) (World Health Organization, 1992).
These criteria were based upon the alcohol dependence syndrome (ADS) concept ofEdwards and Gross (1976), a theoretical formulation of ADS that includes biological, cognitive, and behavioral elements. As illustrated in Table 1, the ICD-10 diagnosis of alcohol dependence is given when three or more of the six criteria are present. Because physiological dependence is associated with greater potential for medical problems (particularly acute alcohol withdrawal), the first two criteria to be considered are tolerance and withdrawal.
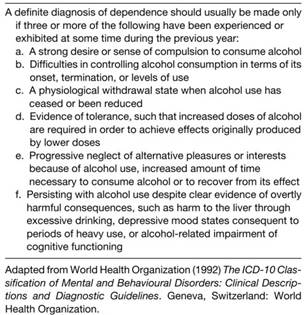
Table 1. Diagnostic guidelines for alcohol dependence syndrome according to the International Classification of Diseases, 10th edition
The remaining criteria reflect the behavioral and cognitive dimensions of ADS: (a) impaired control (i.e., alcohol is consumed in larger amounts or over a longer period of time than was intended; there is a persistent desire or unsuccessful efforts to cut down or control drinking; the individual continues to drink despite knowledge of a persistent or recurrent physical or psychological problem), and (b) increased salience of alcohol (i.e., a great deal of time spent drinking or recovering from its effects; important social, occupational, or recreational activities are given up or reduced due to drinking).
Alcohol withdrawal is a condition that follows a reduction in alcohol consumption or an abrupt cessation of drinking in alcohol-dependent individuals. Uncomplicated cases of alcohol withdrawal are characterized by increased heart rate, elevated blood pressure, hyperthermia, diaphoresis, tremor, nausea, vomiting, insomnia, and anxiety. Onset of withdrawal usually occurs between 4 and 12 h following the last drink. Symptom severity tends to peak around the second day, usually subsiding by the fourth or fifth day of abstinence.
Alcohol withdrawal delirium (also known as delirium tremens) can occur in 5% of cases, usually between 36 and 72 h following alcohol cessation. This condition is characterized by autonomic hyperactivity as well as illusions, hallucinations, psychomotor agitation, cloudiness of consciousness, and disorientation. Prior history of delirium tremens, older age, poor nutritional status, comorbid medical conditions, and history of high tolerance to alcohol are predictors of increased severity of alcohol withdrawal.
In addition to alcohol dependence and alcohol withdrawal, chronic drinking is associated with disturbances in mood, sleep, and sexual function, which are typically included in the diagnostic evaluation. Alcohol-induced mood disorder is characterized by depressed mood and anhedonia, as well as expansive or irritable mood. Although mood disturbances are common among patients entering treatment, alcohol-induced mood symptoms tend to subside within 2-4 weeks following alcohol cessation.
Heavy drinking can also induce generalized anxiety symptoms, panic attacks, and phobias. As with depression, a substantial improvement is of ten observed with abstinence with a full remission of taking as long as 3-4 weeks. Alcohol-induced psychotic disorder is another psychiatric syndrome observed in chronic alcoholics. This disorder is characterized by hallucinations or delusions that usually occur within a month of an alcohol intoxication or withdrawal episode. These psychotic symptoms tend to subside within a few weeks of abstinence, although some patients may require long-term treatment with antipsychotic medication.
Assessment of Alcohol Use Disorders. Improvements in the diagnosis of alcohol use disorders have been facilitated in part by the development of psychiatric and psychological tests. Comprehensive assessment provides the basis for accurate diagnosis and an individualized plan of treatment.
Depending on the severity of alcohol dependence, the nature of comorbid medical and psychiatric pathology, and the presence of family and other social supports, decisions can be made concerning the most appropriate intensity, setting, and modality of treatment. The optimal approach to the assessment of a drinking problem begins with the use of standardized measurement procedures, including screening tests and structured diagnostic interviews.
A number of self-report screening tests have been developed to identify alcoholics as well as persons at risk of alcohol problems. One of the most widely used screening tests is the CAGE (Ewing, 1984), which contains four questions: (1) Have you ever felt you ought to cut (the ‘‘C’’ in CAGE) down on your drinking? (2) Have people annoyed (A) you by criticizing your drinking? (3) Have you ever felt bad or guilty (G) about your drinking? (4) Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover that is, an eye opener (E)? A score of 1 positive response suggests possible alcoholism and a score of two or more is interpreted as definite grounds for further diagnostic evaluation.
The Alcohol Use Disorders Identification Test (AUDIT) is a 10-item screening instrument developed by the World Health Organization for use in primary care settings (Saunders et al, 1993). The AUDIT covers the domains of alcohol consumption, alcohol dependence, and alcohol-related consequences. It has been shown to be sensitive and specific in discriminating alcoholics from nonalcoholics and is superior to other tests in identifying hazardous drinkers. The AUDIT total score increases with the severity of alcohol dependence and related problems and can be used as part of a comprehensive approach to early identification and patient placement.
Following a positive screen or other indications of alcohol problems, diagnostic assessment should be conducted with a standard interview schedule. The alcohol sections of the Composite International Diagnostic Interview (CIDI) and the Structured Clinical Interview for DSM (SCID) provide accurate classification of alcohol use disorders according to both ICD criteria and the criteria contained in the Diagnostic and Statistical Manual of the American Psychiatric Association. An important purpose of clinical assessment is to obtain an estimate of illness severity. The number of ICD symptoms obtained using a structured interview or the total score on the AUDIT screening test can serve this purpose.
Several laboratory tests can be helpful in detecting heavy drinking and assessing its effects on liver function. Tests commonly used by clinicians include serum transaminases, bilirubin, gamma-glutamyl transpeptidase (GGTP), carbohydrate-deficient transferrin (CDT), and mean corpuscular volume (MCV) of erythrocytes.
Diagnostic assessment of people with alcohol dependence also includes measures of family alcohol history, psychopathology, social adjustment, personality disorder, and medical conditions.
Date added: 2024-03-11; views: 753;
