Follicular growth. Follicular Recruitment. Hormone Production from the Follicle
It takes approximately 85 days, or three ovarian cycles, for the development of a preovulatory, or Graafian, follicle from an early preantral follicle. At the onset of this development, a large number of primary follicles are capable of initiating growth. Those that do begin to grow are influenced by many factors, such as age of the woman as well as hormone activity and possibly nutritional status. Only one follicle will eventually become mature, ovulating and releasing the oocyte; the rest will undergo atresia.
The life cycle of a follicle during this 85-day period is shown in Fig. 5. There are eight classes of growing follicles, and at each stage many become atretic. Once the follicle reaches about 0.2 mm in diameter, fluid starts to collect between the granulosa cells. These pockets of fluid grow and merge together to form an antrum, hence the term antral follicle.
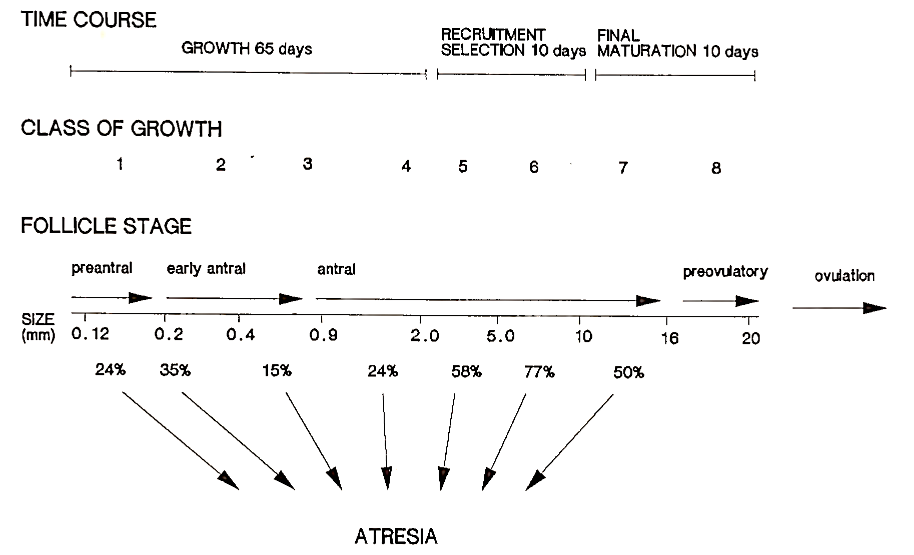
FIGURE 5. Time course of follicle growth. Class 1 is primary, and Classes 7 and 8 are Graafian follicles. At all stages of development, follicles degenerate (atresia). In the human female, only one follicle usually undergoes ovulation each month
A. Follicular Recruitment. After about 65 days of growth, a final cohort of about 15-20 small antral follicles will enter the gonadotrophin-dependent phase of growth. Figure 6 depicts the gonadotrophin and steroid hormone changes that occur during the follicular phase of the human menstrual cycle. The length of the follicular phase is primarily determined by the rate at which the principal antral follicle matures. This follicle exerts its control by secreting hormones that orchestrate the pattern of gonadotrophin release from the anterior pituitary. This process will be addressed in the next section.
If pregnancy does not occur, the corpus luteum regresses, leading to a decline in progesterone levels. Concomitant with this reduction in corpus luteum activity, FSH levels increase. Only those small antral follicles that have acquired gonadotrophin receptors, coincident with this intercycle rise in FSH, will be recruited into the next growth phase.
The most crucial event for the further development of an antral follicle is the activation of the aromatase system by FSH. It is now widely accepted that each small antral follicle (about 4 mm in diameter) has a threshold requirement for stimulation by FSH. This was first postulated by Jim Brown in 1978. Brown’s hypothesis was formulated from the treatment of infertile patients with exogenously administered gonadotrophins of pituitary origin. It was found that the ovary could detect and respond to changes in blood levels of gonadotrophins in the region of 10-30%. Thus, a modest rise in FSH levels is all that is required to initiate the recruitment of antral follicles.
Because follicular development in the human female is highly asynchronous, at the time of the intercycle rise in FSH the ovaries contain a cohort of follicles with varying sensitivities to FSH. The follicle with the lowest FSH threshold will be the first to undergo activation of the aromatase system and begin estradiol production.
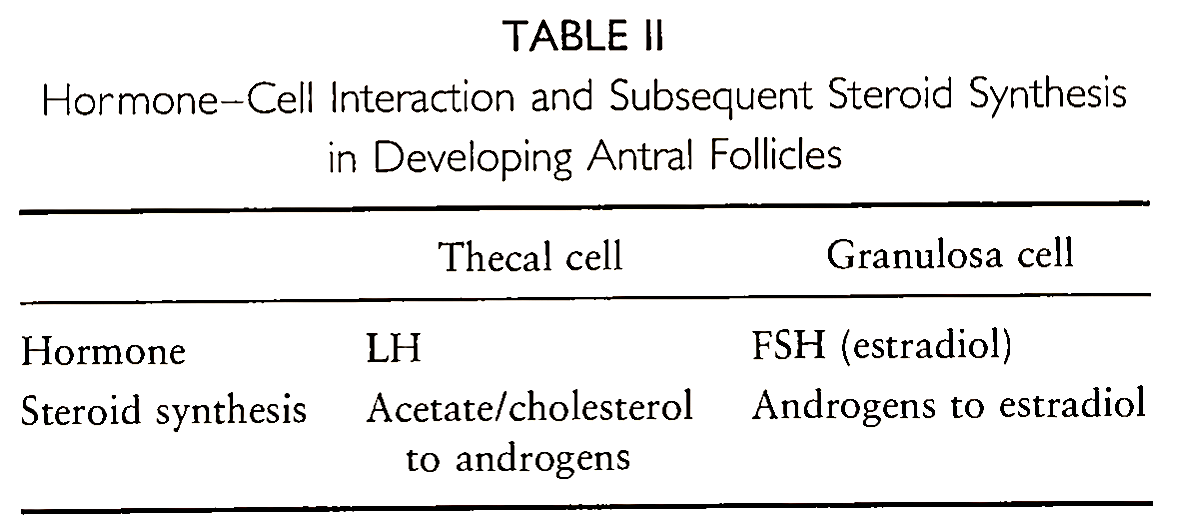
B. Hormone Production from the Follicle. The production of steroids and the increase in follicular size are intimately linked. The proliferation of granulosa cells increases the ability of the follicle to aromatize androgens to estradiol. (The hormone-cell interactions and steroid production of developing antral follicles are summarized in Table II.) This action is a classic example of a positive feedback loop, and it ensures an increasing capacity of the follicle to convert androgens to estradiol, leading to a surge in estradiol production.
The increase in estradiol secretion from the ovary has been demonstrated to have a gonadotrophin-suppressive effect on the hypothalamic-pituitary axis. In particular, FSH secretion begins to decline prior to the midfollicular phase of the menstrual cycle. However, it has been hypothesized that a nonsteroidal factor (inhibin) may also play a role. It was not until the early 1980s that experiments proved the existence of inhibin. These studies involved the use of follicular fluid that contains high concentrations of inhibin-like activity. When injected in vivo, FSH secretion was selectively inhibited.
More recently, inhibin has been purified and shown to be a glycoprotein of about 32,000 molecular weight. It is composed of two subunits linked by disulfide bridges. Inhibin is produced by granulosa cells in response to FSH and androgen stimulation, secreted into the circulation, or concentrated in follicular fluid. However, recent evidence suggests that inhibin does not play a role in the modulation of FSH secretion during follicular development. In the spontaneous menstrual cycle, changes in inhibin concentrations are not related to those in FSH. As we shall see later, inhibin becomes important during the luteal phase.
C. Selection of the Dominant Follicle. It seems, therefore, that FSH secretion in the follicular phase is inhibited by estradiol. The decline in blood FSH levels is in response to increased estradiol secretion from growing follicles. The result of this reduction in FSH during the spontaneous menstrual cycle is the “selection” of one antral follicle, which continues development and ultimately ovulates.
When the fall in FSH occurs, the selected follicle is less dependent on circulating levels of FSH. This is probably because it had the lowest FSH threshold at the onset of the intercycle FSH rise. The follicle will have had longer to activate its aromatase system, leading to higher estradiol production and greater granulosa cell proliferation than its rivals.
Once selected, the follicle is called a Graafian follicle. Selection occurs by about Day 7 of the menstrual cycle. The rest of the cohort of follicles become atretic as FSH is suppressed below their own threshold level.
It is possible to overcome the follicle selection procedure by the administration of exogenous gonadotrophins. After gonadotrophin injections, FSH levels are elevated for a longer time period, thus allowing other follicles to continue development. This principle is practiced in patients undergoing in vitro fertilization treatment. Exogenous gonadotrophins can be given daily throughout the follicular phase of the cycle to promote “superovulation.”
Another physiological process concerning selection may also contribute to the emergence of a dominant follicle. Rising levels of estradiol, in conjunction with FSH, induce the appearance of LH receptors on the outer layer of granulosa cells. Thus, there is a gradual change in distribution for gonadotrophin receptors, which may be critical for further follicular development. In vitro studies have shown that granulosa cells possessing both FSH and LH receptors responded identically to both hormones in terms of aromatase activity and steroid production. This may mean that the presence of both LH and FSH receptors on granulosa cells may further protect the emerging dominant follicle from declining FSH concentrations.
Date added: 2022-12-11; views: 903;
