Cells and Molecules Involved. Arachidonic Acid Metabolites
Historically, the hallmark of acute inflammation in tissues has been the demonstration of extravascular accumulation of fluid and plasma components, the intravascular activation of platelets, and the presence of polymorphonuclear leukocytes in the tissues. Should the response proceed to a more chronic phase, the cellular accumulation involves monocyte/macrophages, lymphocytes, eosinophils and mast cells, and plasma cells. Each of these cells has a primary role to play in the body’s response to challenge, and the progression from an acute to a chronic response is seen as a continuum, rather than the responses being distinct entities.
Arachidonic Acid Metabolites. Recent advances in our understanding of the acute phase response have involved the discovery and characterization of the chemical and peptide mediators that the body uses to communicate with and regulate the cellular participants in the response.
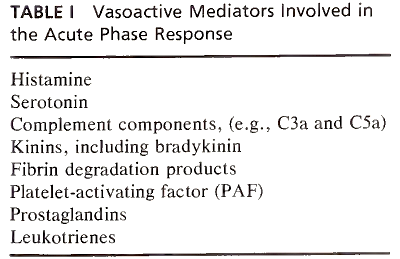
These molecules include various vasoactive compounds that immediately alter vascular permeability:
- preformed mediators such as histamine and serotonin;
- fragments from the activation of the plasma biochemical pathways of inflammation, including the complement components C3a and C5a, bradykinin and other kininlike factors of the kallikrein pathway, and the products of fibrin degradation of fibrin-split products;
- elements of phospholipid metabolism, including platelet-activating factor;
- and products of the metabolism of arachidonic acid, including the prostaglandins and leukotrienes (Table I).
Of the vasoactive compounds, the factors generated by the action of phospholipase A2 or C and released arachidonic acid have immediate and far-reaching consequences in the tissues. The actual mechanism depends on both the specific mediator and the tissue being affected. Most cells of the body, whether activated and mobile leukocytes or activated/stimulated stromal cells, release these mediators.
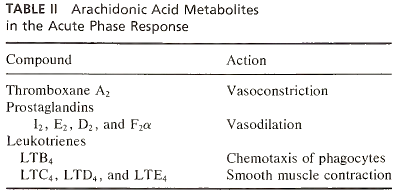
Metabolism of arachidonic acid by cyclooxygenases results in the formation of thromboxane A2 and other prostaglandins, while metabolism by lipoxygenases results in the formation of leukotrienes and a family of hydroperoxyeicosa-tetraenoic and hydroxyeicosatetraenoic acids. The metabolites have both stimulatory and inhibitory effects on the activation of inflammatory and stromal cells. Moreover, depending on the organ involved, major physiological changes result, such as bronchoconstriction and bronchodilation in the lung. Relevant to the acute phase response is the action of leukotriene B4 as a potent chemotactic agent for leukocytes (Table II).
Following tissue injury there is immediate vasoconstriction followed by vasodilation, resulting in increased blood flow to the tissues, which is the cause of the redness and warmth associated with the local acute phase response. The most prominent acute feature involves endothelial cell contraction and the opening of the gap junction between the cells, exposing the basement membrane.
This increase in vessel permeability, particularly at the postcapillary venules, results in an increase of fluids and plasma components accumulating in the tissue, peaking about 30 minutes after tissue injury. Within the tissue the accumulation is referred to as edema, while subepithelial accumulation results in blister formation. Sometimes the fluid accumulation coincides with bacterial and leukocyte presence, resulting in the formation of pus.
The increased permeability caused by some metabolites, coupled with the chemotactic action of others, represents a coordinated mechanism for the accumulation of leukocytes at tissues involved in the local acute phase response. Pain appears to be associated with the generation of molecules such as bradykinin upon activation of kallikrein action on kininogen during the clotting cascade.
Date added: 2023-05-09; views: 809;
