Peripheral blood. Types of peripheral blood cells
Blood is a unique connective tissue in that the extracellular matrix forms a circulating fluid compartment called plasma (55% by volume) in which are suspended the cellular elements (45% by volume). The fluid plasma compartment contains proteins (i.e., globulins, albumins, fibrinogen, and assorted enzymes), hormones, metabolites, various salts in solution, and colloidal substances such as chylomicrons in dispersed form. The extracellular matrix of typical connective tissues usually contains formed connective tissue fibers such as collagen or elastin; however, in peripheral blood, fibrous proteins are not normally formed unless clotting has initiated the polymerization of the soluble monomeric blood protein, fibrinogen, into insoluble fibrin fibers. Serum is equivalent to plasma after removal of fibrinogen and other elements of clotting.
The cellular elements of blood include erythrocytes (red blood cells), leukocytes (white blood cells), and circulating cytoplasmic fragments known as platelets, all of which are formed by hemopoiesis in bone marrow and lymphoid tissues. Red blood cells are anucleate biconcave disks that mainly function within the cardiovascular system through their efficient transport of oxygen and carbon dioxide to and from different tissues/ organs in the body. Platelets are cytoplasmic fragments derived from megakaryocytes, and like red blood cells, they are anucleate. They play an important role in the clotting of blood and also serve as the source of platelet- derived growth factor, an important cytokine in the body.
Two distinct categories of white blood cells have been identified based on their nuclear morphology and the presence of characteristic specific granules within their cytoplasm. The first category, agranular or mononuclear leukocytes, includes lymphocytes and monocytes, which possess round or slightly indented nuclei and small lysosomes known as azure granules. Lymphocytes can be subdivided into two important groups based on their function. T lymphocytes are long-lived cells involved in cellular immunity, including delayed hypersensitivity, graft rejection, and, for some antigens, the modulation of antibody responses. Subsets of T cells regulating these processes are referred to as T helper cells, T suppressor cells, cytotoxic T cells, and memory T cells. В lymphocytes are primarily involved in humoral immunity and are responsible, after appropriate stimulation, for the formation in various tissues of plasma cells that secrete immunoglobulins.
Monocytes circulate for brief periods in peripheral blood and then migrate into tissues where they differentiate into macrophages. Their primary role is the phagocytosis and digestion of microorganisms or substances recognized as nonself, as well as the processing of antigens for stimulation of immunocompetent lymphoid cells. The monocyte may also give rise to actively phagocytic cells distributed throughout the body, known as the mononuclear phagocytic system (i.e., connective tissue macrophages [histiocytes], foreign body giant cells, Kupffer cells, alveolar macrophages, peritoneal macrophages, microglia, osteoclasts, and free or fixed macrophages in lymphoid tissues).
The second category of white blood cells are the granular leukocytes, which have lobulated nuclei and specific granules in their cytoplasm that stain with components of the Romanovsky-based stains and from which these cells draw their names (neutrophils, eosinophils, and basophils). Neutrophils are also known as PMNs (polymorphonuclear cells) because of the presence of two to five nuclear lobes. Specific granules of neutrophils contain lysozyme, lactoferrin, collagenase, and bactericidal cationic proteins, while the azure granules (lysosomes) found in most white blood cells contain acid hydrolases, myeloperoxidase, lysozyme, elastase, and neutral proteases. Neutrophils play a major role in bacterial phagocytosis.
Eosinophils contain a complex group of substances in their specific granules including acid phosphatase, arylsulfatase, histaminase, beta-glucuronidase, cathep- sin, phospholipase, eosinophilic peroxidase, major basic protein, and RNAase. Eosinophils are drawn into connective tissue by factors released by mast cells during allergic reactions and parasitic infections. The eosinophil neutralizes agents secreted by mast cells (i.e., leu- kotrine C, histamine), thereby modulating the allergic reaction enhanced by mast cells, and also participates in the phagocytic disposal of antigen-antibody complexes formed in allergic responses, such as hay fever or asthma.
Basophils contain specific granules rich in heparin, histamine, chemotactic factors for eosinophils and neutrophils, leukotrines, platelet-activating factor, and enzymes capable of degrading connective tissue elements. These cells, like mast cells, have immunoglobin E bound to receptors on their surface, and immunologic triggering of them results in secretion of specific granules leading to immediate hypersensitivity reaction. In its extreme form this is referred to as anaphylactic shock.
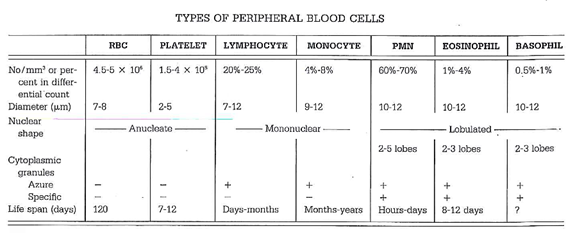
The differential count in peripheral blood, size, shape, cytoplasmic characteristics, and life span of the different blood cells are shown in the following table.
Date added: 2022-12-11; views: 955;
