Diseases Leading to Elevated Triglycerides
Familial Combined Hyperlipidemia. Familial combined hyperlipidemia (FCHL) is one of the most common inherited lipid disorders. The prevalence data suggest the disorder affects 1 to 2% of the population. It has traditionally been defined as an autosomal dominant trait, but more recently has been considered an oligogenic disorder with variable penetrance. It presents with a variable phenotype and affected individuals have lipid profiles that may fluctuate from one reading to the next and may present with high LDL-C, high TGs, or both.
It has been said that when a patient has multiple lipid profiles that are different, suggesting laboratory error, FCHL should be suspected. Affected relatives can present with elevated LDL-C while others present with elevated TGs and still others have both. The disorder is associated with a marked increased risk for ASCVD. Though the disease appears to be inherited in an autosomal dominant manner, it is likely that multiple genes may be responsible for the lipid disorder. Certain mutations in the genes for lipoprotein lipase (LPL), ApoA5, ApoE, and ApoC3 have been implicated.
The single-nucleotide polymorphism (SNP) rs3737787 has been associated with differences in the expression of the target genes for upstream transcription factor 1(USF1) in adipose tissue and lymphoblasts, as well as higher TG concentrations in certain populations, and is the SNP most consistently associated to FCHL. Genomewide association studies have revealed that patients with FCHL have high polygenic lipid scores for associated LDL-C and TG variants consistent with a polygenic origin for the disorder.
The increased risk for coronary disease likely stems from increased production of very low- density lipoprotein (VLDL), due to increased ApoB production or decreased clearance of ApoB-containing lipoproteins, leading to increased atherogenic particles as well as small dense LDL particles (Fig. 3.3).
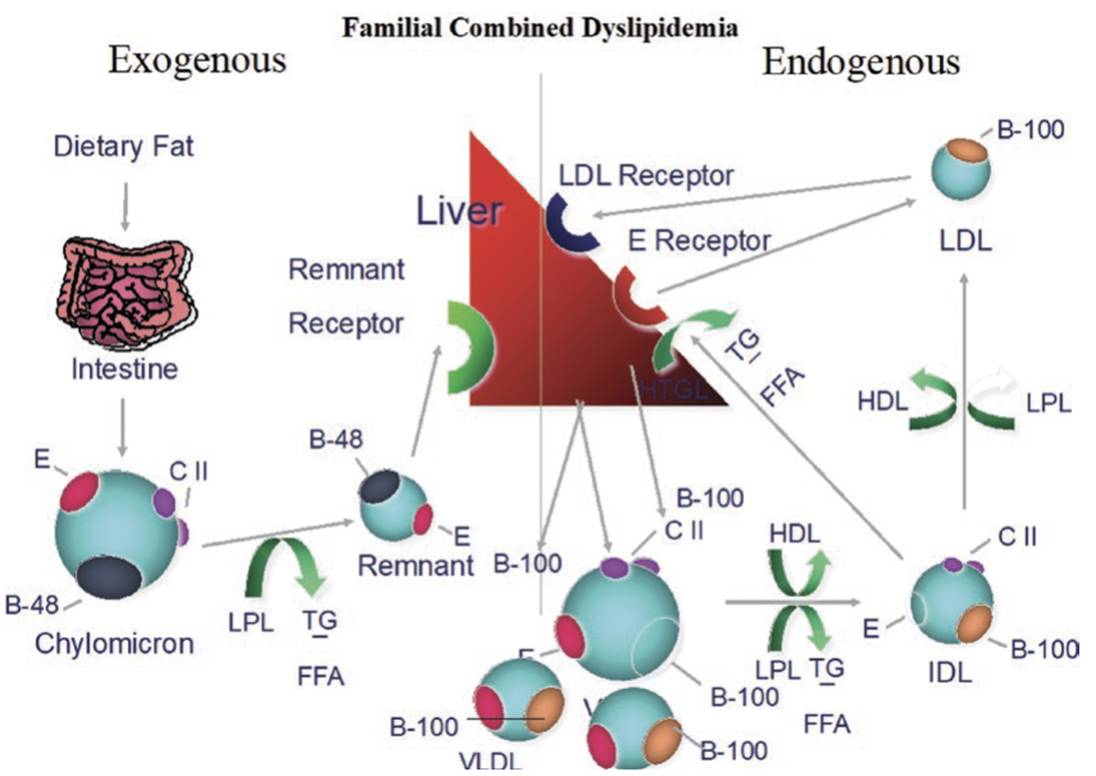
Fig. 3.3. Familial combined dyslipidemia is an autosomal dominant disorder characterized by an overproduction of ApoB leading to increased numbers of atherogenic lipoproteins. Some individuals may present with high levels of VLDL while others may have increased LDL. Family members therefore can have elevated LDL-C, elevated TG, or both, in their lipid profiles
The disorder tends to develop in adolescence, which helps to differentiate it from FH or familial chylomicronemia syndrome (FCS), both of which are evident from childhood. The dyslipidemia is exacerbated by secondary causes, such as obesity and diabetes mellitus, and patients with FCHL have a high incidence of concomitant insulin resistance and development of type 2 diabetes. Patients with FCHL have been shown to have common pathophysiological mechanisms with type 2 diabetes. These include muscle and adipose tissue insulin resistance, as well as impaired insulin-mediated suppression of hepatic production of VLDL.
The diagnosis is suspected if one first-order relative has markedly elevated lipid levels, whether LDL-C, TGs, or both. Commonly, there is a strong family history of premature CAD. The LDL-C levels do not achieve the level seen in FH, and the TG levels, though often elevated, are not as high as those seen in FCS. CAD, though common in FCHL, is relatively rare in patients with FCS and familial hypertriglyceridemia, where the primary morbidity for the latter two is pancreatitis. Because FCHL is not a pure monogenic disorder, the role of genetic testing is not extremely helpful at present, but helps to rule out other causes of dyslipidemia. Elevated ApoB levels support the diagnosis, with ApoB levels usually greater than simultaneously obtained LDL-C levels in these patients.
Treatment of this FCHL includes aggressive control of secondary causes starting with a low carbohydrate and low saturated fat diet, as well as statin therapy to reduce the risk of CVD. Abstaining from alcohol and smoking, and management of obesity are also necessary. A 5% weight loss in patients with FCHL has been shown to significantly reduce TG and non-HDL-C levels in 3 to 6 months. Statins are first-line therapy for these patients because of the markedly elevated risk for CAD. If TGs are significantly elevated despite diet and statin therapy, the addition of omega-3 fatty acids and/or fenofibrate is some times necessary for control of TG levels. It is also very important to aggressively control secondary disorders such as diabetes mellitus.
Date added: 2025-02-17; views: 362;
