Geographic Distribution of HIV/AIDS. Epidemiology and Transmission
Within about a decade of being identified as a new disease and epidemic in 1981, it was clear that HIV had already spread around most of the world. At the same time or soon after, it was clear that different regions and countries had different rates of HIV prevalence and different patterns of infection within their populations. Sub-Saharan Africa clearly has the highest rates, and an epidemic that is spread by heterosexual transmission and the vertical transmission of HIV from infected mothers to their infants.
The initial epidemics in the United States and Europe were largely due either to rectal sex among homosexual men or to blood exchange among injection drug users. Hemophiliacs and blood transfusion recipients were also infected at the earliest stages, but by the mid-1980s most blood for medical use was successfully screened.
It is estimated that about 6% of adults are currently infected in sub-Saharan Africa, a rate that is about 10-fold higher than the United States, Asia, Western Europe, or Latin America (see Table 1). North Africa has much lower rates, about 0.2%. Within sub-Saharan Africa, the region of southern Africa has the highest rates, with about 20% of adults infected. In some places, such as Swaziland, Botswana, or the KwaZulu-Natal region of South Africa, more than one-third of all pregnant women may be infected. The epidemic in southern Africa did not appear to undergo rapid expansion until the 1990s, which was later than for other regions of Africa.
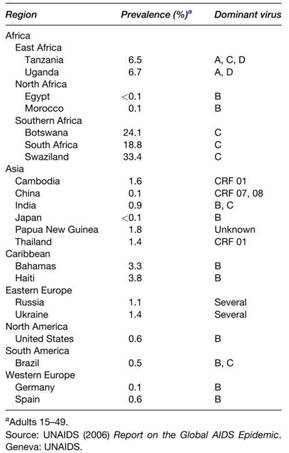
Table 1. Representative prevalence rates for HIV in different regions of the world, 2005
The epidemic appeared to expand first in Central and East Africa, and subsequently in West Africa are about average for sub-Saharan Africa, while rates in Central and West Africa are below those in the rest of sub-Saharan Africa.
The epidemics are caused by different viruses. In southern Africa, it is HIV-1 subtype C, which appears to undergo genetic variation even faster than the others. In East Africa, both HIV-1A and HIV-1D are common. In Central and West Africa, the predominant virus is CRF 02 A/G. In Northern Africa, where rates are so low, it is HIV-1B, the same virus that predominates in the United States and Europe.
In Asia, rates are generally low. In China and Japan, they are 0.1% or lower, and the predominant virus is HIV-1B or recombinant viruses with components of both B and C. The highest rates in Asia are in Papua New Guinea (1.8%), Cambodia (1.6%), Thailand (1.4%), and India (0.9%). The virus linked to the regional epidemic in Cambodia, Thailand, and Myanmar is CRF 01 A/E. Multiple viruses are associated with the epidemic in India. After Africa, the next highest rates are in the Caribbean, particularly in Haiti (3.8%) and the Bahamas (3.3%) (see Table 1).
Russia and Ukraine now have rates that exceed 1%. Latin America has an overall rate of about 0.5%, which is also the rate in Brazil, one of the largest countries that had an aggressive response to the epidemic in the early stages.
Epidemiology and Transmission. Most transmissions in sub-Saharan Africa are due to vaginal sex (see Table 2). Virus is detectable as both free virus particles and cell-associated proviral DNA in semen and vaginal fluids. Because younger women seem to have sex with older men much more often than older women have sex with younger men, rates in young adults are usually much higher in women. While overall rates are higher in women than in men, this is particularly true for those at ages 16-24, where four or five times as many women may be infected.
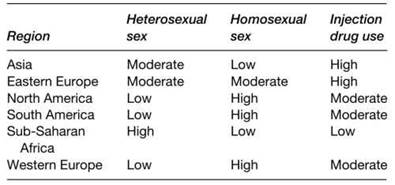
Table 2. Relative importance of different mechanisms for HIV transmission
Coinfections with other sexually transmitted diseases, particularly herpes, appear to enhance the sexual transmission of HIV. Some viruses, such as HIV-1C, may also have enhanced tropism for cells that line reproductive tract surfaces, such as Langerhans cells in the foreskin of the penis and at the vaginal-cervical junction.
Transmission by rectal sex is more important for homosexual transmission. The recipient of insertional sex seems to be at greatest risk. Injection drug use transmission with dirty needles is still a major problem in many regions of the world, including Thailand, China, Eastern Europe, Latin America, and the United States. While transmissions with whole blood are now unusual, careful screening is still not done in some regions of the world, and even with proper antibody screening a few infectious blood units are tested and used after the donor has become infected but before the development of antibodies.
When large fractions of women are infected, as in many countries in Africa, there are many opportunities for infants to become infected by vertical transmission. Except during the periods of late pregnancy, birth, or breast-feeding, children are not at risk of infection until they become sexually active. Infants who are infected HIV-negative at birth using PCR but positive when tested at 1 month of age are listed as having become infected while passing through the birth canal.
This is clearly an operational definition, as infants who become infected during the last days before birth or during the first few days of breast-feeding would be categorized as having become infected at the time of birth. Although merely operational - based on broad time intervals, and thus mechanistically inaccurate - this definition has provided a useful reference to compare interventions that may block mother-to-infant transmission.
When infants test PCR-negative at 1 month of age and positive some time later, the infant is classified as having become infected during breast-feeding. This obviously assumes that breast-feeding has occurred and the infant was not exposed to blood by transfusion.
From 20-45% of infants born to HIV-positive mothers may become infected, with the higher numbers more likely to occur when breast-feeding is practiced. In most situations in Africa, breast-feeding is practiced, and the risk of infection continues as long as breast-feeding has gone on, at least for periods of up to two years.
The largest number of infections, perhaps 40-60%, occur during the time of birth, with about 15-20% occurring in utero and 25-40% occurring while breast-feeding. However, these percentages vary in different situations and may vary with the HIV subtype as well. For HIV-2, only about 1-2% of infants become infected after being born to positive mothers.
Date added: 2024-03-11; views: 553;
