Pathogenesis and Natural History
Infections that occur via sexual transmission almost always involve an HIV classified as having the CCR5 co-receptor pattern of tropism. In the case of most HIV-1 subtypes, particularly B and D, this often results in the evolutionary selection of a different co-receptor phenotype, CXCR4, in the infected individual. For the first week or two, virus replication appears to be restricted to local tissues such as lymph nodes, and the individual would not be categorized as infected using standard antibody screening tests.
The virus infection then spreads to blood lymphocytes, monocytes, and analogous cells in systemic lymph nodes. Although less than 1% of blood lymphocytes are infected, much larger numbers of cells are infected in lymph nodes. At the early stages, up to a few weeks after infection, high levels of virus are usually present in blood (i.e., viremia), but the person is still not detected as HIV-infected using antibody tests alone (see Figure 4).
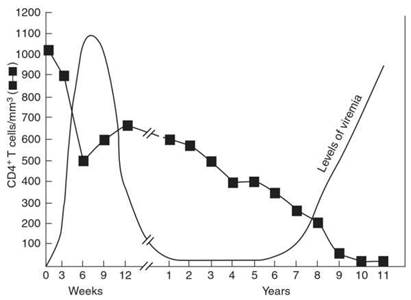
Figure 4. Typical course of HIV infection
At this stage, infection would be detectable using PCR or antigen tests. The infected individual is also highly infectious, by both sexual transmission and blood transfusion (where the blood would have been scored as negative if antibody tests alone were used).
During the stage of acute viremia, the numbers of CD4 lymphocytes also fall, though a partial recovery is seen as soon as the virus load level goes down. This stage is also characterized by a rapid rise in levels of antibodies, which can then serve as a tool for diagnosis of infection, at least until the very late stages of clinical AIDS.
Very few infected individuals develop sustained clinical signs or symptoms until several years later, although the acute stage of infection may be associated with ‘flu-like’ symptoms that soon get resolved. Although almost all develop clinical AIDS after 8-10 years, a very small fraction become ‘long-term nonprogressors’ who exhibit no signs or symptoms for up to 15-20 years.
The signs and symptoms, whenever they occur, are normally associated with reduced levels of CD4 T lymphocytes and immune suppression. When symptoms of clinical AIDS are apparent, the actual disease manifestation is associated with the degree of immune suppression. Thrush, caused by Candida albicans, is often one of the first things observed.
Outcomes such as pneumonia due to Pneumocytis carinii or meningitis due to Cryptococcus neoformans only occur at late stages, after the immune system is largely destroyed. Tuberculosis is a common outcome in all parts of the world, especially in Africa, and a wasting syndrome and Kaposi sarcoma are also common in Africa.
Date added: 2024-03-11; views: 681;
