Soil Microorganisms: Antibiotic Discovery and Resistance Mechanisms
The soil environment hosts a complex food web characterized by intricate interactions between diverse organisms. These entities constantly engage in predation and competition for limited resources. In response, a vast array of biological processes for both attack and survival have evolved over millennia. One such strategy is the deployment of chemical substances, effectively a form of biochemical warfare. Notably, when isolated, some of these compounds possess potent medicinal properties for humans, chief among them being antibiotics (Fig. 4.20).
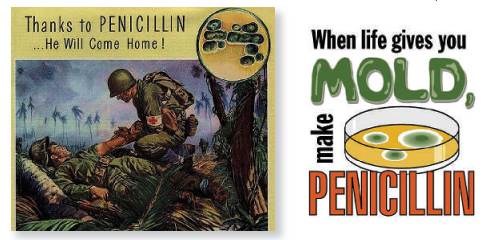
Fig. 4.20: Penicillin antibiotics are historically significant because they were the first drugs that were effective against many previously untreatable diseases and infections. Although still widely used, many types of bacteria are now resistant to penicillin
Several foundational antibiotic classes were discovered through the isolation of compounds from soil-dwelling organisms. The classic example is penicillin, isolated from the fungus Penicillium chrysogenum. Furthermore, critical aminoglycosides like streptomycin and kanamycin, along with tetracyclines, were derived from soil actinomycetes. Another important group, lipopeptides such as daptomycin, also originate from Streptomyces, a genus of filamentous bacteria within the actinomycete group.
Antibiotics are systematically categorized based on their primary effect on target microorganisms. Bactericidal antibiotics directly kill bacteria, while bacteriostatic agents impair and inhibit microbial growth without immediately causing cell death. This fundamental distinction influences their clinical application and dosing regimens. Each class exerts its effect by disrupting specific, vital cellular processes in the competing microbe.
The mode of action varies significantly between antibiotic classes, explaining their selective toxicity. For instance, penicillin and related beta-lactams attack and inhibit the synthesis of the bacterial cell wall. In contrast, aminoglycosides and tetracyclines disrupt protein synthesis by binding to ribosomal subunits. An organism's susceptibility depends entirely on whether it possesses the specific cellular target the antibiotic is designed to disrupt, a principle central to antimicrobial therapy.
A critical phenomenon observed both in nature and clinical settings is antibiotic resistance. While problematic in medicine, its precedents are deeply rooted in the soil environment. Soil microorganisms are perpetually exposed to a cocktail of natural compounds, including antibiotics produced by neighbors. This exposure creates intense evolutionary pressure, selecting for individuals with inherent or acquired resistance mechanisms to survive.
Conversely, antibiotic-producing organisms, such as Streptomyces, must possess intrinsic resistance mechanisms to avoid self-destruction by their own metabolic products. Therefore, the soil represents a vast, ancient reservoir of genetic information on resistance. Studying this natural laboratory provides invaluable insights into underlying biochemical processes, potentially guiding strategies to circumvent or delay the emergence of new clinical resistance.
Research reveals that evolution has pushed soil microbial adaptability even further. Certain microorganisms not only tolerate multiple antibiotics but can also utilize these compounds as a sole carbon source, effectively consuming them as food. This demonstrates a remarkable level of biochemical versatility, highlighting that human antibiotic use is merely intersecting with a pre-existing, dynamic natural process of chemical interaction and adaptation.
Resistance emerges because antibiotics apply a powerful selective pressure on a microbial population. Individuals possessing a resistance factor, whether through mutation or acquired genes, survive and reproduce. Those lacking the factor are eliminated. Once established within a single bacterium, the resistance determinant can disseminate rapidly across a population and even between different species through horizontal gene transfer (HGT).
Horizontal gene transfer operates through three primary mechanisms, allowing for the lateral exchange of DNA containing antibiotic resistance genes within a single generation. Transformation occurs when a competent bacterium takes up free DNA fragments released into the environment from a lysed, dead neighbor. This DNA may then be incorporated into the recipient's genome, conferring new traits.
A second mechanism, transduction, involves bacteriophages (viruses that infect bacteria). Occasionally, during viral replication, phage particles mistakenly package host bacterial DNA, including resistance genes. When this phage infects a new bacterial cell, it injects this genetic material, potentially altering the recipient's genetic makeup. This viral vector facilitates gene transfer between often-distantly related microbes.
The third key process is conjugation, often described as bacterial "mating." Here, two bacteria form a direct physical connection via a pilus. Through this conduit, mobile genetic elements like plasmids or fragments of chromosomal DNA are transferred from the donor to the recipient cell. Conjugation is a highly efficient and promiscuous process, capable of transferring resistance genes across genus and species boundaries.
The combined action of transformation, transduction, and conjugation means a novel resistance mechanism need only evolve once in a single soil bacterium. From that point, it can potentially spread throughout an entire microbial community. This natural exchange network in soil pre-dates clinical antibiotic use and underscores why resistance is a formidable, naturally occurring challenge that medicine must continuously address through prudent antibiotic use and innovative research.
Date added: 2025-12-15; views: 99;
